Selling to Health Plans Isn’t Enough. Members Also Have to Use It.
Landing a health plan contract isn’t the same as getting members to engage. This article breaks down how to build for adoption from day one.
Upward Growth provides health tech leaders with the playbooks and proof to transform complex markets into real growth. Each week, we deliver clear, practical strategies on positioning, messaging, and growth, so leaders can close enterprise deals and build repeatable momentum.
🤝 Work with Ryan on payor growth strategy: Contact me
🟦 Connect with the author, Ryan Peterson, on LinkedIn.
💡 Newsletter sponsorships are available: Learn More
A friend of mine recently texted to celebrate his company’s first major health plan contract. They’d spent nine months selling their digital health solution into a regional Blues plan, and finally, the SOW was signed.
“We finally landed them,” he said.
I shared with him the same thing I’ve said for years:
“You didn’t land the fish. You just got your fishing license.”
It’s a useful analogy in digital health. A fishing license gives you permission to try, but no promise of a catch. And too many vendors confuse access with adoption. Getting through procurement doesn’t mean you’ve achieved traction. It just means you now have the opportunity to prove your value, and sadly, many vendors don’t.
Most vendors don’t succeed because they never really built a plan for what happens after the contract. Their teams were hyper-focused on getting the contract, and less on driving member behavior, assuming the health plan would take it from there. It rarely does.
This article breaks down:
Why vendors get stuck at “live but irrelevant”
What health plans expect after the contract is signed
How to bake adoption into your go-to-market before the deal closes
The Most Common Mistake: Assuming Coverage = Adoption
“2.6 million covered lives” sounds impressive. So does landing a top-tier health plan.
But those numbers don’t matter if no one uses your product.
Most members have no idea what’s covered, and the plan isn’t going to market your product for you. If your logo is just one among dozens in the benefit catalog, how do you expect to stand out, let alone get selected?
It’s like getting into a grocery store. You’ve earned shelf space, but you’re buried on the bottom row, competing with house brands, and no one’s sampling your product. Visibility doesn’t equal velocity.
On the other hand, the plan considers its job done once you’re listed in their benefit portal. From that point on, no one is thinking about your product. If you want members to use your product, you can’t wait until go-live to figure that out. The vendors who break through are already shaping adoption during the sales process.
Four Moves That Actually Drive Member Adoption
Getting listed in a benefit catalog doesn’t create behavior. Most vendors stall out post-contract because they never figured out how adoption would actually happen.
The plan won’t drive it for you. Their internal teams are focused on compliance, care delivery, and core operations. They’ll add you to the portal. Maybe mention you in a newsletter. But really, that’s often the extent of the lift. The rest is on you.
The vendors who gain traction walk into the sales process already knowing what member adoption requires internally and externally, and have come prepared.
(Once you start winning member adoption, the next challenge is turning that early traction into account growth. Here’s how to do it: You Landed the Account. Here’s How You Grow It.)
But first, you have to solve the adoption problem itself. Here are four moves the best teams build in long before go-live:
1. Tie Member Usage to a Metric That Matters
Plans don’t promote benefits just because they’re helpful. They promote what they’re accountable for.
If member adoption of your product doesn’t help improve a tracked metric, like something the plan is already being evaluated or funded against, you might get listed, but you won’t get surfaced. You need to connect member usage to plan-level pressure. That’s what earns airtime.
Examples:
A musculoskeletal program that reduces avoidable ED visits from falls or back pain
A behavioral health tool that improves access scores tied to CAHPS
A nutrition benefit that supports chronic condition control for Stars adherence
A care navigation solution that reduces DSNP churn by improving first-call resolution
And it’s not enough to vaguely say, "We help with Stars."
The best vendors don’t just align to a metric. They turn it into a wedge. Something specific, time-sensitive, and politically safe to act on. That’s what gets internal teams to prioritize adoption and push your benefit forward.
Better move: Identify the metric you support, the department that owns it, and the specific pain or gap that makes your solution easier to activate than ignore.
2. Appoint Someone Who Owns Adoption
Often, vendors treat member adoption as a post-sale problem. Sales owns the deal. Implementation owns setup. Customer Success owns the relationship. But rarely does anyone own whether members actually use the product.
Step back and think how strange that is.
You’re trying to drive behavior in a population that doesn’t know your name, doesn’t trust unfamiliar brands, and often doesn’t even know the benefit exists. Being listed in a health plan catalog doesn’t create credibility. Only you can do that (and it’s a never-ending job).
That’s why you need a dedicated owner for member activation. Someone like a Client Activation Lead, Growth Programs Manager, or Plan Success Partner. This role is designed to work across teams, drive adoption before go-live, and stay accountable for member adoption and usage.
Their job should include:
Building relationships with operational leaders inside the plan
Identifying how and where your product gets surfaced to members
Securing activation paths before go-live
Tracking usage trends and escalating when engagement stalls
Gathering feedback directly from members and frontline staff
Better move: Create and fill a role explicitly accountable for member usage. If no one owns activation, don’t expect traction. Expect churn.
3. Anchor to Real-World Member Moments
Too often, outreach is disconnected from when the member actually needs help. The plan pushes generic benefit reminders. Vendors send passive nudges. Rarely does it drive action, especially if the timing is off or the context is missing.
Adoption happens when your benefit shows up in a real moment, like when the member is confused, stuck, or trying to solve a “right now” problem. Not when they’re skimming a newsletter or browsing the portal. You need to anchor your product to specific, operational moments in the member journey. That means tying into workflows the plan already runs.
Examples:
A care gap call that surfaces your product for chronic pain
A nurse line script that flags your service based on symptoms
A discharge summary that includes your mental health tool as part of follow-up
A denied claim notice that points the member to your benefit as an alternative
And these distribution channels are most effective if you map them before go-live and hand them to the health plan, ready to deploy.
Better move: Identify the 3 to 5 real-world member moments where your product is immediately relevant. Then show up to the sales process already embedded in those workflows, complete with drill-down reporting and member-level ROI metrics to back it up.
4. Treat Adoption Like a Funnel
Vendors often show up with good intentions and the standard tools: collateral, benefit emails, staff trainings, and maybe even a kickoff webinar. But without structure, sequencing, or accountability, those efforts are ignored or fade fast. Adoption most frequently stalls because no one owns what to do when it’s not working.
A real campaign doesn’t rely on passive awareness. It is sequenced over time. It assigns owners. It defines what success looks like and what happens when usage stalls. It treats member adoption like a funnel, with stages, signals, and interventions, not a one-time announcement.
This approach also fosters internal trust. Plan stakeholders can see the structure, while operational teams know when and how to reinforce it. Early signals, such as low click-throughs or lagging activation, are treated as cues to adjust, rather than being buried in quarterly reviews.
Examples worth building in:
Pre-launch messaging sent through trusted plan channels like care management or pharmacy
Triggered outreach tied to member events, like an ED visit or new diagnosis
Weekly usage dashboards with defined thresholds that trigger follow-up
Recurring reviews with the plan team to assess uptake and reinforce support
Better move: Show up with a rollout campaign that makes adoption visible and accountable. Don’t just support launch. Lead it, with a timeline, owner map, and a game plan to adapt when traction lags.
Final Thought
The hardest part isn’t getting listed, it’s getting used.
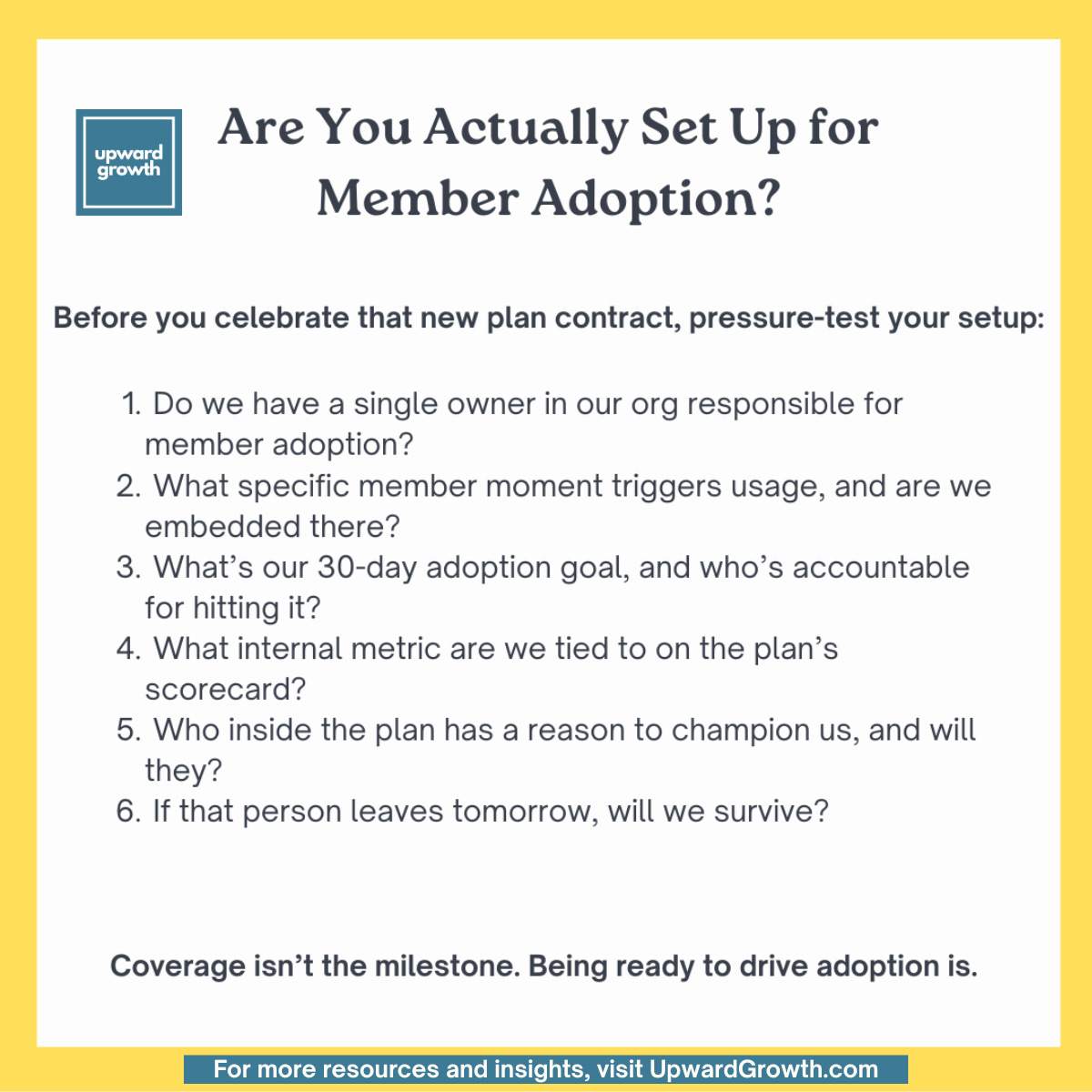
Member adoption doesn’t happen by accident. It happens when vendors treat it as a core part of their go-to-market strategy: with an accountable owner, clear KPIs, embedded member touchpoints, and a campaign that doesn’t end at go-live.
You got the license. Now prove you can land the fish.
🔒 Like This? Upgrade to a paid Subscription.
The free newsletter covers the big ideas. Paid subscribers get the full breakdowns, including client-tested strategy, behind-the-scenes examples, and deeper thinking you won’t find anywhere else.
→ [Become a Paid Subscriber]
About the Author
Ryan Peterson writes Upward Growth, where he shares practical insights on selling health tech into the payor market. With 15+ years in healthcare growth leadership, he focuses on helping vendors translate their value into traction with health plans.
🟦 Connect with him on LinkedIn.