Five Health Tech Trends That Will Shape Sales Cycles in 2026
What's changing in how health plans evaluate and select vendors, and how to adjust your GTM accordingly.
Upward Growth provides health tech leaders with the playbooks and proof to transform complex markets into real growth. Each week, we deliver clear, practical strategies on positioning, messaging, and growth, so leaders can close enterprise deals and build repeatable momentum.
🤝 Work with Ryan on payor growth strategy: Contact me
🟦 Connect with the author, Ryan Peterson, on LinkedIn.
💡 Newsletter sponsorships are available: Learn More
Today’s Upward Growth is brought to you by…Ellevate
The executive search firm that health tech vendors call when they need client-facing talent
Ellevate fills sales, marketing, and account management roles for health tech companies selling to payers, providers, and employers. From early-stage startups to established vendors, we find the commercial leaders who can close.
We also help experienced sales executives and CEOs find board and advisory seats with PE/VC firms and health tech companies.
Hiring for your team or exploring board opportunities? Let’s talk.
[Schedule a Call with Ellevate]
Last week, I published my year-end scorecard on the five trends I predicted for 2025. I got four right and one wrong. More importantly, the exercise clarified something about where this market is headed.
The through-line from 2025 could be distilled to health plans are de-risking their vendor relationships. And that isn’t changing heading into the New Year. However, the way that de-risking shows up in buyer behavior is still evolving. Because health plans aren’t just asking for more proof. They’re asking harder questions about which vendors will survive the next two years, which solutions address problems they’re required to solve versus problems they’d like to solve, and whether the ROI shows up in this contract year or depends on assumptions about next year’s Stars bonus.
What I’m seeing across dozens of sales conversations is that buyers now require a level of clarity most vendors aren’t providing. Clarity about what you solve. Clarity about who you serve. Clarity about what you can actually prove.
This article covers five trends that will shape the GTM environment in 2026. They aren’t predictions about what might happen. They’re patterns already underway.
Before I get into each one, here’s why they hang together and why you should read this regardless of what line of business you serve, or whether you sell to payors, providers, or employers.
Government-sponsored healthcare operates as an interconnected system, even when vendors focus on a single line of business. Regulatory pressure in one program often migrates to another. For example, buyer scrutiny that starts with Medicaid MCOs eventually shows up in MA plan procurement. And innovation that works in commercial self-funded employers gets tested in Medicare (And vice versa). If you only sell to MA plans, you still need to understand what’s happening in Medicaid and the ACA marketplace, because those dynamics travel. These five trends reflect that interconnection. Some will hit your business directly. Others will hit your buyers, your competitors, or your future market.
Trend 1: Health Plan Buyers Are Asking New Questions About Vendor Stability
The headline numbers look healthy. Digital health VC hit $9.9 billion through Q3 2025, exceeding the same period last year. But beneath the surface, the market structure is shifting in ways that affect every vendor, regardless of stage or funding status.
The Series B market has collapsed. Only 30 companies reported Series B rounds through Q3 2025, compared to an average of 60 per year over the past three years. The median time between Series A and Series B has increased to 27 months, up from 17 months two years ago. Meanwhile, mega-rounds are concentrating capital among a smaller number of well-funded winners, and 35 percent of 2025 rounds are “unlabeled,” often signaling companies that raised at pandemic valuations and now need cash but can’t justify a priced round.
Here’s why this matters even if your own funding situation is stable: health plan buyers have noticed. They’ve been burned by vendors that folded mid-implementation or couldn’t invest in product improvements after the initial sale. Procurement teams are asking harder questions about financial stability. RFPs increasingly include requirements around runway and funding status. The due diligence that used to focus on clinical outcomes and integration capability now includes a serious look at whether you’ll still be operating in two years.
This dynamic creates both risk and opportunity. If you’re well-funded, you can win deals partly by emphasizing stability and long-term partnership when competitors can’t credibly make that case. If you’re at an earlier stage or navigating a difficult fundraising environment, you need to proactively address buyer concerns about durability before they become objections. That might mean highlighting capital efficiency, customer retention, or strategic backing. It might mean being selective about which deals you pursue, so you’re not overextending. The worst response is to ignore the concern and hope buyers don’t ask.
The broader point is that the funding environment has changed buyer psychology. Health plans are thinking about vendor risk differently than they were two years ago, and your GTM needs to account for that regardless of where you sit in the funding landscape.
Trend 2: Prior Auth Compliance Creates a Finite Buying Window
Most regulatory deadlines don’t create true forcing functions. Compliance timelines slip, enforcement is inconsistent, and buyers find workarounds. But occasionally a deadline arrives with enough weight to create a genuine must-buy moment, and every vendor should understand how to recognize and position around these windows, whether the regulation touches their business directly or not.
Prior authorization in 2026 is a clear example. The CMS Interoperability and Prior Authorization Final Rule requires Medicare Advantage plans, Medicaid, and CHIP to implement a FHIR-based API for prior authorization by January 1, 2026. Plans must allow providers to query PA requirements and submit requests electronically. Expedited decisions must happen within 72 hours, standard decisions within 7 days. Specific reasons for denials must be provided through the API.
What makes this a real forcing function rather than another deadline that slips? CMS has signaled serious enforcement. Plans have internal pressure beyond regulatory requirements, since prior auth is one of the most complained-about aspects of health insurance. The technical lift is real, and build-versus-buy timelines favor buying for anything going live in 2026. Prior auth automation investment grew 10x year over year in 2025. Plans are moving.
If you’re a prior auth solution provider, this is your moment, and your 2026 pipeline should reflect that. But even if prior auth isn’t your core business, the dynamic matters. Adjacent vendors in care management, utilization management, and provider engagement can identify integration opportunities to ride the compliance spending wave. Platform and data companies can position themselves around the new data flows these APIs create. And every vendor can learn from watching how this plays out: which companies captured the window, which missed it, and what set them apart.
Regulatory forcing functions are rare. When they happen, they reward vendors who recognized the moment early and positioned themselves accordingly.
Trend 3: Policy Chaos Is Splitting Health Plan Buyers Into Three Camps
Health plan buyers are under financial pressure across every line of business right now. But they’re not all responding the same way. What I’m seeing is that buyers are splitting into three distinct camps based on their financial position and risk tolerance, and most vendors aren’t qualifying for these differences.
Defensive buyers are pulling back on anything discretionary. These are plans with thin margins, recent losses, or direct exposure to policy changes that threaten their economics. If your product doesn’t address a regulatory requirement or an immediate cost crisis, you’re deprioritized. They’re not taking meetings on “nice to have” solutions.
Opportunistic buyers are doing the opposite. Plans with strong balance sheets and growth ambitions see this as a chance to gain ground while competitors are frozen. They’re accelerating investments in member acquisition, retention technology, and operational efficiency. These buyers are moving faster than normal because they’re playing offense, while others are playing defense.
Compliance-driven buyers continue to purchase regardless of conditions. Prior authorization deadlines, interoperability requirements, and quality measure performance don’t pause for policy uncertainty. If your solution addresses a regulatory must-have, these buyers are still active.
The pressure creating this segmentation is real and widespread. Medicaid is facing $1 trillion in federal funding cuts from the recently passed reconciliation bill. MA plans are navigating margin compression, benefit pullbacks, and market exits. Commercial plans are bracing for cost increases not seen in 15 years. And in the ACA marketplace, 22 million Americans face premiums that could double after enhanced subsidies expired at year-end. A discharge petition will force a vote on a three-year extension in January, but the outcome remains uncertain.
If your primary market is Medicare Advantage, you might wonder why ACA or Medicaid dynamics matter to you. They matter because (as we said earlier) the financial pressure in one line of business often changes how a plan operates across all of them. A plan losing money in Medicaid may tighten vendor budgets enterprise-wide. A plan exiting the ACA markets may redirect resources to MA. The buyers you’re calling on are often making decisions in the context of their entire book of business (or at least their entire budget), not just the segment you sell into.
Your 2026 pipeline includes all three camps of buyers, so make sure you’re addressing them uniquely. The qualification question that matters most right now: “How is your organization responding to the current policy environment? Accelerating or pulling back?” That single question tells you which camp you’re selling into and whether the deal is worth pursuing on your current timeline.
Trend 4: Healthcare Costs Are Pushing Employers to Buy Differently
Every working American is talking about rising healthcare costs. Premiums are climbing. Deductibles are climbing. And employers, who cover the majority of insured Americans through self-funded plans, are feeling the pressure acutely. Group health plan costs are projected to rise 8 to 9 percent in 2026, the steepest increase in over a decade.
This pressure is driving employers to look beyond their traditional health plan relationships for solutions. Sixty-three percent of covered workers are now in self-funded plans, in which employers bear the risk directly. Seven percent of firms with 50 or more employees contract directly for primary care services outside their health plan networks. Thirty percent have contracts for virtual primary care. ICHRA adoption has increased 1,000 percent since 2020, with projections for 5.8 million covered lives by 2026.
For health tech vendors, this raises a strategic question many are debating: Should we expand from selling to health plans to selling to employers, or vice versa?
The answer isn’t obvious, and it depends on your product, your sales motion, and your willingness to build for a different buyer. Health plan buyers and employer buyers operate on different priorities, different timelines, and different proof points. Health plans care about PMPM cost, MLR, Stars scores, and regulatory compliance. Employers care about total benefits spend, employee satisfaction, and retention. Health plans have multi-year contract cycles and complex decision committees spanning clinical, network, IT, compliance, and finance. Employers often move faster but renew annually, and decisions typically run through HR and finance.
Vendors who try to sell to both channels with a single GTM motion usually underperform in both. The sales cycles and the proof points are different. And the decision-makers care about different things. A vendor who walks into an employer meeting with health plan collateral, talking about HEDIS measures and Stars performance, is speaking a language the buyer doesn’t use. The same is true in reverse: an employer-focused vendor that tries to sell to an MA plan without understanding how MLR pressure and risk-adjustment economics shape purchasing decisions will lose to competitors who do.
The question isn’t whether employer revenue is attractive. It’s whether you’re willing to build a second GTM motion, with dedicated positioning, dedicated proof points, and potentially dedicated sales resources, or whether you’ll accept underperforming in the channel you’re not designed for. From my experience, half-committing usually produces worse results than picking a lane and going all-in.
But even if you’re not planning to expand into a new channel, understanding these dynamics matters. Healthcare is consolidating and converging. M&A happens, and suddenly you need to know how the other side of the market works. Finally, career opportunities emerge in adjacent spaces too, and so the more you understand about how healthcare costs flow through the system, the more future job opportunities you’ll have open to you.
Trend 5: Outcomes Claims Without Reproducible Evidence Are Getting Ignored
Health plan CFOs have become the hidden gatekeepers for vendor decisions. Clinical champions still matter, but finance increasingly controls whether deals move forward. And CFOs evaluate outcome claims differently from clinical buyers.
The problem is that most vendors are still leading with outcomes narratives rather than outcomes evidence. “We improve medication adherence.” “We close gaps faster.” “We reduce avoidable utilization.” These claims have become so common that they’ve lost meaning. When every vendor says some version of “we improve outcomes,” buyers stop hearing it.
What I’m seeing in competitive deals is that winners have shifted from narrative to evidence. Not “we improve adherence” but “12 percent reduction in 30-day readmissions for CHF patients in a 50,000-member MA population, measured via claims data over 18 months, validated by an independent actuarial firm, and replicated across three implementations.”
That level of specificity is what CFO scrutiny now requires. Defined population. Clear timeframe. Transparent methodology. Statistical validity. Reproducibility across multiple customers.
The Hinge Health and Omada Health IPOs earlier this year illustrate what this looks like at scale. Both companies spent over a decade building clinical evidence before going public. Their outcomes claims weren’t marketing. They were validated, reproducible, and sufficiently specific to withstand investor due diligence and public-market scrutiny.
You don’t need a decade and hundreds of millions in funding to start building an evidence stack. But you do need to treat outcomes measurement as infrastructure, not an afterthought. That means consistent methodology across implementations, tracking the same metrics the same way, so results are comparable. It means being honest about what you can prove and what you can’t, rather than overclaiming and hoping buyers don’t ask hard questions. And it means investing in data pipelines and validation relationships that enable you to generate credible evidence over time. I’ll go into more detail on how to build this in the coming weeks.
The gap between vendors with this evidence and those without is widening. Buyers have seen too many one-off results that don’t replicate. Single case studies might generate interest, but reproducible evidence is what closes deals.
Final Thought
2025 was about health plans de-risking their vendor relationships. 2026 is about what happens after the bar has been raised. Buyers are now screening vendors for financial stability before evaluating your product. Regulatory windows are compressing timelines and concentrating spend. Policy chaos is segmenting buyers in ways that break one-size-fits-all sales motions. The employer channel is demanding its own GTM, not a repurposed health plan pitch. And outcomes claims that worked three years ago are getting ignored because everyone makes them, and no one can prove them.
These aren’t five separate challenges. They’re five angles on the same shift: health plan and employer buyers are making fewer bets, and the vendors who win those bets will be the ones who’ve done the positioning, qualification, and evidence work before the conversation starts.
Over the next several weeks, I’ll go deeper on each trend. How to position around it, how to sell into it, and what vendors who are getting it right are doing differently.
A personal note: This is the last Upward Growth article of 2025. I’ve published every Tuesday since mid-January, and so I’m taking next week off to recharge (no article) before Year Two kicks off on January 6th, 2026.
Finally, two requests have come up repeatedly over the past few months:
Audio versions of these articles - something you can listen to in the car or at the gym instead of reading.
A podcast or video format - with more commentary on current events and what they mean for health tech growth strategy.
I’m seriously considering both. If you have thoughts on what you’d want from either format, reply to this email or reach out on LinkedIn.
Thanks for reading this year. See you in 2026! 🎉
Ryan Peterson
Principal
Upward Growth
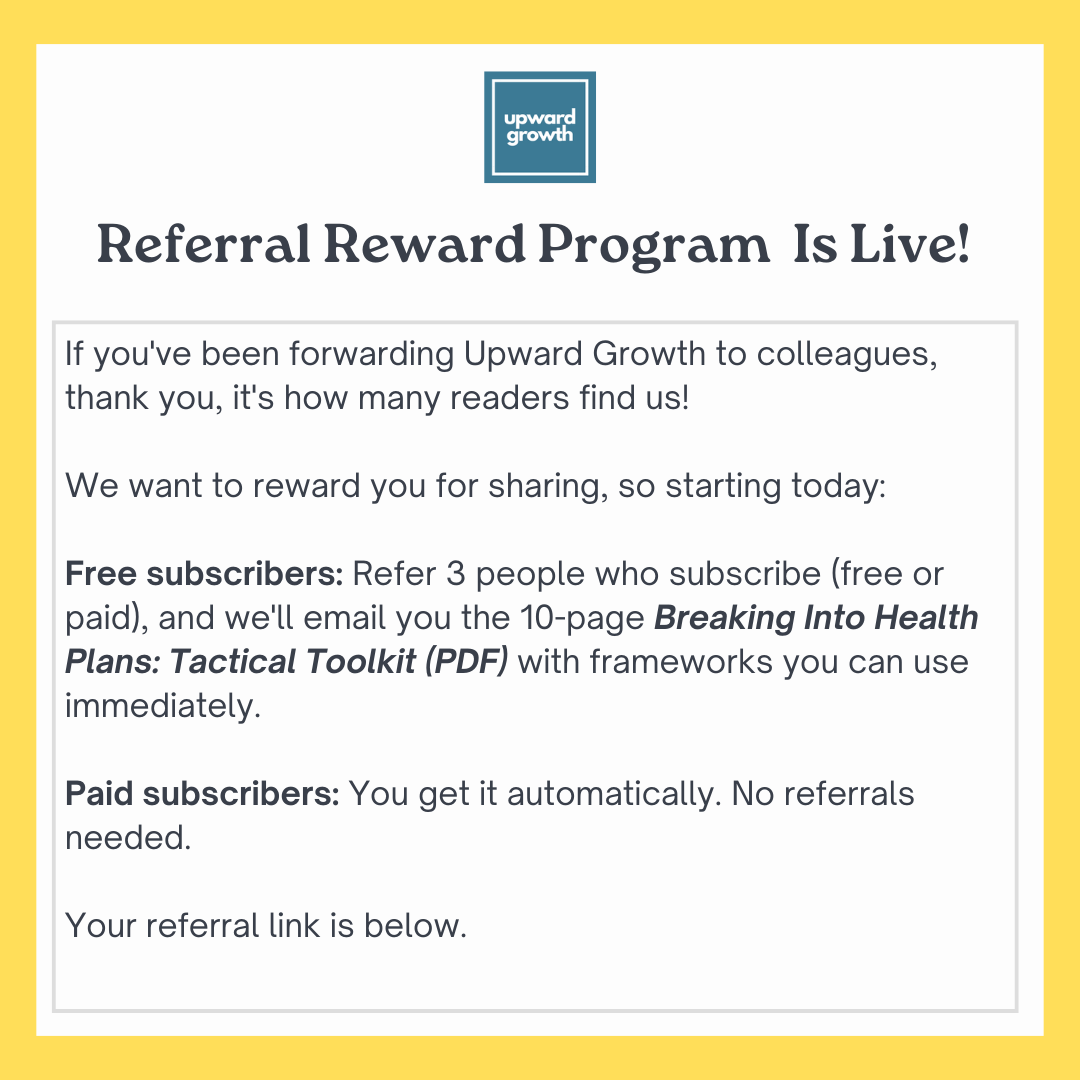
Click the button above to get your personal referral link. When 3 people subscribe using your link, I’ll email you the Tactical Toolkit.